According to electronic health records company Epic, telehealth visits in the U.S. in July accounted for 21 percent of total encounters, down from 69 percent in mid-April during an early peak of the health crisis. Several factors contributed to the surge, including the Centers for Medicare & Medicaid Services (CMS) expanding the list of covered telehealth services, issuing temporary waivers and loosening restrictions; healthcare consumers reluctant to make in-person visits, reduced provider office hours, and an increase in electronic consultations in lieu of direct care.
Despite the drop between April and July, the surge in telehealth visits that preceded it shows that telehealth helped fill an unprecedented void and was a viable short-term option for many healthcare consumers, with the trend expected to continue. One market research report forecasts a global $55.6 billion telehealth market by 2025, up from $25.4 billion in 2020.
The recent decline in telehealth visits does indicate, however, that in many cases there is no substitute for in-person care. This is especially true for colorectal, cervical, and breast cancer screenings and other preventive measures that contribute to Health Effectiveness Data and Information Set (HEDIS) scores.
Closing Care Gaps In Healthcare is Top of Mind
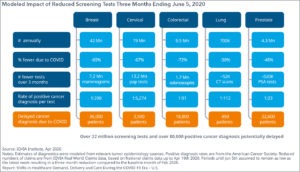
The below graphic showcases the cost of reduced screening tests in stark terms of a delayed cancer diagnosis. As the first column shows, there was a 69 percent reduction in breast cancer screenings for a three-month period ending early June, representing 7.2 million fewer tests (of 42 million annually). At a standard 1:200 rate of positive cancer diagnosis per test, that equates to 36,000 patients delaying a cancer diagnosis as a direct result of a delayed screening because of the pandemic.
Early breast cancer diagnosis, as with another cancer diagnosis, results in higher survival rates, more treatment options, and reduced costs.
The pandemic also has had a significant impact on managing chronic conditions such as diabetes, COPD, and hypertension. According to a Wellfleet study from June of roughly 1,000 patients with a chronic condition, 57 percent said they delayed receiving healthcare due to the pandemic, either at their own discretion or their doctor’s. With approximately 60 percent of all U.S. adults managing at least one chronic condition, that represents tens of millions of delayed visits.
Not surprisingly, in a separate survey of healthcare providers from Definitive Healthcare, the impact of delayed care was cited by 24.4 percent of respondents as one of the largest emerging trends, second only to losses sustained due to the cancellation of elective surgeries (36 percent). Interestingly, these trends overtake the two biggest trends of 2019 – industry consolidation and the growing influence of healthcare consumerism – as being top of mind for providers.
Orchestrate a Personalized Healthcare CX Journey
Providers generally follow a three-pronged strategy for closing care gaps: quality scorecards, population health management, and patient engagement. While many organizations have identified quality metrics and have population health initiatives underway to satisfy the first two pillars, most fall short of their full potential, as they are missing the third leg of the stool: effective patient engagement. Metrics and reporting are simply not enough.
Effective patient engagement that helps reduce gaps in care requires more than just knowing a healthcare consumer’s medical history – or compiling patient data relevant for quality metrics reporting or managing broader population health. It also requires knowing – at an individual consumer level – a consumer’s risk tolerance for an in-person visit, their means for engaging with a telehealth option (if available), access to transportation and other social determinants of health, current health condition, and other risk factors. But knowing all this still does not bring the healthcare consumer into the clinic or the doctor’s office. There is also the matter of maximizing appointment scheduling by optimizing engagement with the healthcare consumer. Will an SMS directly from a provider that notifies a member of a gap in care result in a confirmed appointment better than an email or call? Can you offer a day and time that works best with the member’s schedule? Creating a relationship with a healthcare consumer to drive better outcomes requires having every conceivable piece of consumer data in one place.
We’ve covered the emergence of healthcare consumerism and the implications of increasingly dynamic healthcare consumer journeys amid industry uncertainty in previous blogs here and here. Alleviating pent-up demand for healthcare services throughout the pandemic poses yet another significant challenge for healthcare payers and providers who struggle to help consumers manage a frictionless healthcare experience.
Demand for unmet services and care illustrates the crucial need for payers and providers to understand the needs of their patients. Without that full understanding, it becomes difficult if not impossible to address those needs by orchestrating a personalized experience that reduces a consumer’s fear and anxiety and increases the positive impact a payer/provider can have on individual health outcomes.
The pandemic exacerbates the challenge to provide a holistic healthcare experience, exposing long-standing, built-in operational inefficiencies in the healthcare system caused by disparate data and an implicit tolerance for friction. Until Covid-19, an unintegrated network of payers and providers and a fractured, confusing, and often frustrating experience by the end consumer were chalked up as routine hurdles. A pent-up demand raises the stakes; with the real human and economic costs of delayed care, payers and providers no longer have the luxury of accepting the status quo.
Improve the Healthcare CX with a Single View of the Consumer
Improving health outcomes – in this case, closing higher-than-usual care gaps – requires that healthcare providers and payers have a single view of the healthcare consumer. To engage a consumer in the channel of his/her preference with a next-best action that recognizes, in real-time, the consumer’s current situation presupposes that there be no data siloes; claims and clinical data, for instance, must be integrated with everything there is to know about the healthcare consumer.
A single view provides stakeholders with the full understanding of a consumer, ensuring that healthcare professionals always engage in the right channel, at the right time, and with the right content or message – at every point in the consumer’s healthcare journey.
Doing this at scale for hundreds of thousands or millions of healthcare consumers requires automated machine learning (AML), with self-training, code-free models that do not have to be taken offline every time a desired outcome or metric changes. With AML, healthcare professionals can easily test the efficacy of every previous outreach, using the results to optimize all subsequent interactions without having to rely on data scientists, human judgment, or trial and error.
One Platform for a Personalized Experience
Customers in the healthcare industry are using the Redpoint rg1 digital experience platform to intelligently orchestrate personalized experiences, at scale, to drive better outcomes. One, for example, not only has integrated claims and clinical data but is also plugged into a provider’s scheduling system so an optimized interaction includes letting a consumer know – in real time – appointment options that fit with a consumer’s availability. If one provider’s office or clinic has long wait times, the healthcare consumer is notified of another nearby provider that may have more capacity. The notification even includes an estimated drive time from the consumer’s location.
This type of personalized healthcare experience may seem simplistic, but many healthcare payers and providers lack this capability; consumer marketing that builds relationships with individual consumers is rarely prioritized, especially in fee-for-service payment models that incentivize volume. Establishing a meaningful relationship by personalizing a holistic experience throughout a healthcare journey removes many of the traditional barriers to improved health outcomes.
Taking the view that devoting resources to building out this capability somehow interferes with operations or traditional marketing efforts is short-sighted. With so much now at stake with an unexpected and concerning widening of care gaps, healthcare marketers must adopt a new approach that prioritizes the healthcare consumer’s experience. A single view is a starting point to improve outcomes, lower costs and improve overall satisfaction.
Related Content
Survey Says: Healthcare Personalization Has Room to Grow
Clear the Hurdles for a Personalized Customer Experience
A Personalized Customer Experience Delivers Loyalty
Be in-the-know with all the latest customer engagement, data management, and Redpoint Global news by following us on LinkedIn, Twitter, and Facebook.
